
Things are not always as obvious as they seem
Haniyah, living with BBS
Haniyah has Bardet-Biedl syndrome (BBS), a rare melanocortin-4 receptor (MC4R) pathway-related disease, and has been in front of you the whole time.
Like other patients with an undiagnosed rare MC4R pathway disease, Haniyah spent years struggling with insatiable hunger (hyperphagia), which led to her developing obesity at a young age and putting her at elongated risk of life-threatening obesity complications.1,2
She was able to get the support she needed when her doctor re-evaluated her symptoms, recognised the clinical features and then urgently referred her for genetic testing.
Undiagnosed adults with BBS face significant long-term risk of potentially life-threatening complications observed in general obesity, in addition to the other challenges of BBS-specific features1,3,4
BBS is a rare MC4R pathway-related disease and can present in many ways2,5,6
Due to the many genetic variants involved in BBS, there is no ‘typical’ patient. Clinical features vary in severity – some patients may have many clinical features, and some may have less.2,6
However, hyperphagia and resulting obesity are two of the earliest and most distressing symptoms of BBS.7
It's important to be aware of all the clinical features of BBS, so that you can make a thorough clinical assessment.2
Rare Clues
Can you find all the clues to make a correct BBS diagnosis?
Looking beyond the obvious
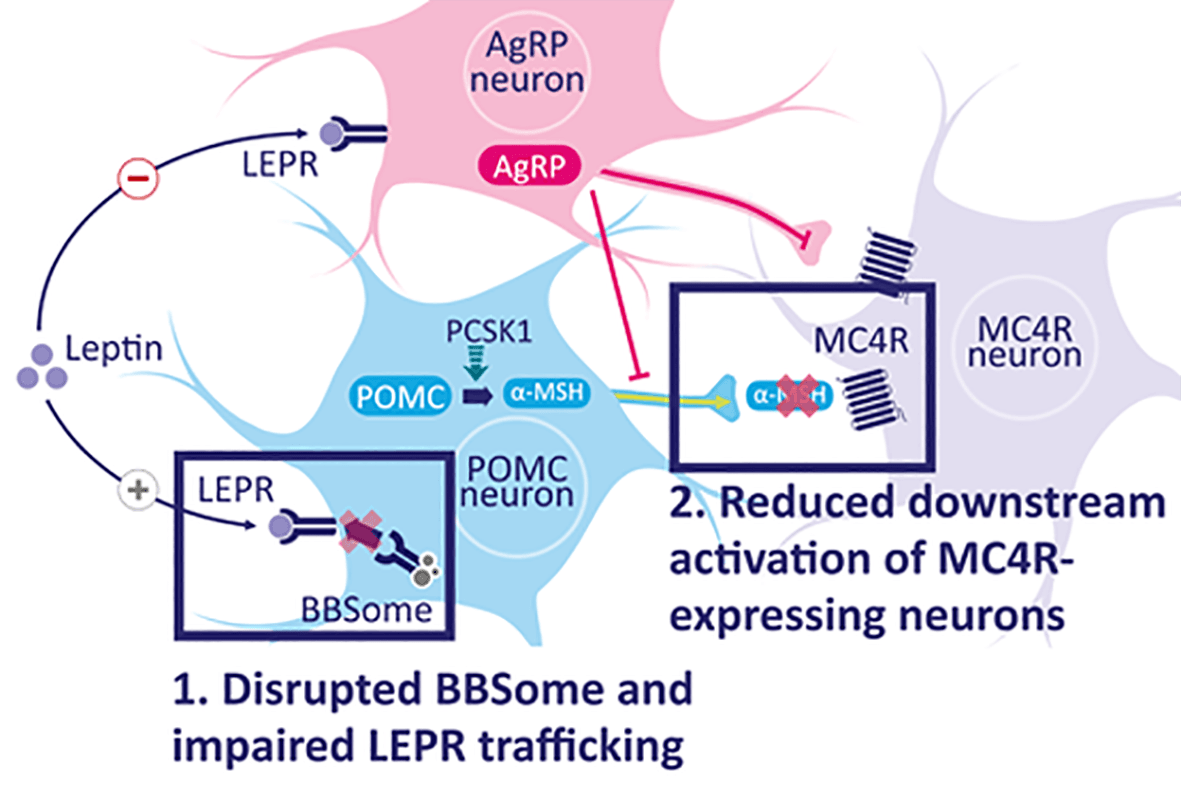
The MC4R pathway
Learn more about the mechanism of the MC4R pathway, and how impairment can lead to hyperphagia and early-onset obesity in BBS.
The right genetic test can bring clarity for you and your patients8
Reviewing Haniyah against the 2024 ERN consensus statement and recommendations confirmed that she had several of the primary clinical features for BBS – so her endocrinologist referred her for a genetic test.2
Genetic testing with the correct gene panels was crucial for her differential diagnosis, which meant she could get the multi-disciplinary support she needed.2,8
Obesity in BBS can be early-onset and progressive2
Like for many other patients with BBS, Haniyah’s diagnosis came late, but it was essential to getting her the tailored support she needed.9
Undiagnosed adults face significant long-term risk of potentially life-threatening complications observed in general obesity, in addition to the other challenges of BBS-specific features.2,3,4
Acting quickly is critical, as the correct diagnosis can enable tailored management strategies and improved patient outcomes.2
Re-evaluate. Recognise. Refer.
By re-evaluating the clinical features of BBS, recognising the root cause of your patients’ hyperphagia and early-onset obesity and referring for genetic testing, you can help identify the presence of BBS, and move patients onto the appropriate care path with the co-ordinated support of a multi-disciplinary team.2,9
Think back to your patients with a long-term history of obesity - could they be living with an undiagnosed rare neuroendocrine disease?
If you recognise signs, consider immediate referral for genetic testing.
Got a specific question?
If you can't find what you're looking for, or want to discuss a topic in more detail, reach out to our team.
References:
- 1. Lister NB, et al. Nat Rev DIs Primers. 2023;9(1):10.1038/s41572-023-00435–4
- 2. Dollfus H, et al. Eur J Hum Genet. 2024;32(11):1347–1360
- 3. Choquet, H, Meyre, D. Genome Med 2. 2010;2(36)
- 4. Wrzosek M, et al. Obes Surg. 2018;28(12):3902–3909.
- 5. Forsythe E, et al. Orphanet J Rare Dis. 2023;18(1):182
- 6. Forsythe E, et al. Front Pediat. 2018:6:23.
- 7. Forsythe E, et al. Eur J Hum Genet. 2013:21:8–13
- 8. Malhotra S, et al. J Pediatr Genet. 2021;10;194–203
- 9. Huvenne H, et al. Obes Facts. 2016;9:158–173