Hyperphagia and Obesity in bardet-Biedl syndrome is a Growing concern
UNCOVERING A ROOT CAUSE OF THE GROWING CONCERN
A growing
concern
Genetic variants in the melanocortin-4 receptor (MC4R) pathway can impair the regulation of hunger, food intake, satiety and energy expenditure. This can lead to hyperphagia (pathological, insatiable hunger) and a decreased energy expenditure, resulting in early-onset obesity, regardless of environmental and lifestyle factors.3,4
The root cause of early-onset obesity is often underdiagnosed. Access to appropriate tools and proactive identification of clinical features can help aid diagnosis and move those living with a rare MC4R pathway disease, onto their appropriate care path.3
Got a specific question?
If you can't find what you're looking for, or want to discuss a topic in more detail, reach out to our team.
Understanding hyperphagia in patients with Bardet-Biedl syndrome
Dr Forsythe discusses the impact of hyperphagia on patients of all ages with Bardet-Biedl syndrome and their caregivers as well as the approach to patient care.
Rhythm Pharmaceuticals is leveraging a IQVIA's Healthcare Professional Authentication solution to identify your eligibility to access this video content. If you already have an IQVIA account using it with other healthcare providers, please click 'Login' otherwise click 'Signup'.
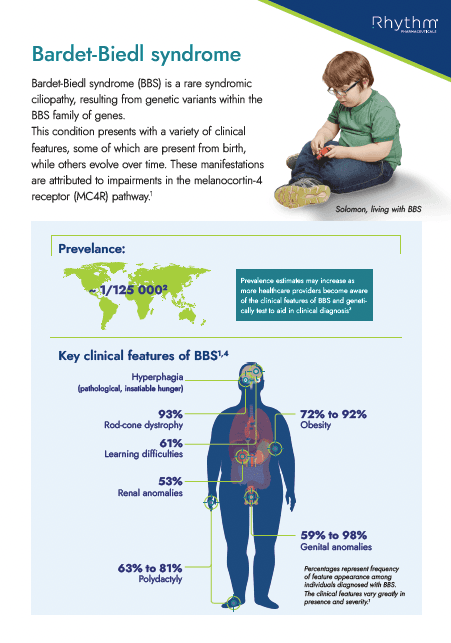
Primary and Secondary clinical features
BBS is a rare MC4R pathway disease characterised by a range of clinical features, such as rod-cone dystrophy, that evolve over time. Obesity (present in 72-92% of patients) and hyperphagia are among the most distressing manifestations of BBS, with a substantial burden on patients and caregivers.4,5
Additional clinical features include:4,6,8
Primary clinical features:
- Genital anomalies
- Learning difficulties
- Obesity
- Polydactyly
- Renal anomalies
- Rod-cone dystrophy
Secondary clinical features:
- Anosmia or hyposmia
- Ataxia or poor coordination
- Brachydactyly or syndactyly
- Dental anomalies
- Developmental delay
- Diabetes mellitus
- Hepatic fibrosis
- Left ventricular hypertrophy or congenital heart disease
- Mild spasticity (especially lower limbs)
- Polyuria or polydipsia
- Speech delay or speech impairments
- Strabismus, cataracts, astigmatism
Despite the urgent need for early diagnosis to reduce the impact of future comorbidities, significant delays exist in BBS diagnosis due to lack of awareness and the slow emergence of certain clinical features.7
Learn about treatment
For patients with genetic obesity, time is ticking

Genetic
confirmation
Variants in at least 26 genes have been identified and are known to cause BBS.7 Clinical guidelines recommend genetic testing to inform diagnosis and appropriate interventions in patients with the clinical features of hyperphagia and early-onset obesity. A genetic diagnosis of BBS can make a significant difference to an individual's life by:8,9,10
- Improving access to appropriate care for hyperphagia and early-onset obesity
- Reducing the social stigma of obesity and providing coping strategies for managing stigmatisation
- Empowering the individual and carers to understand the root cause of their condition and make informed decisions about their care
- Allowing for preventive or prophylactic screening of associated conditions
Content Hub
Click here to find additional information on rare MC4R pathway diseases as well as educational resources and meetings produced by Rhythm.
We will continue to update this page with resources about BBS as well as other rare diseases of the MC4R pathway.
Educational information about Bardet-Biedl syndrome (BBS), its association with obesity, characteristics and route to diagnosis
Handout
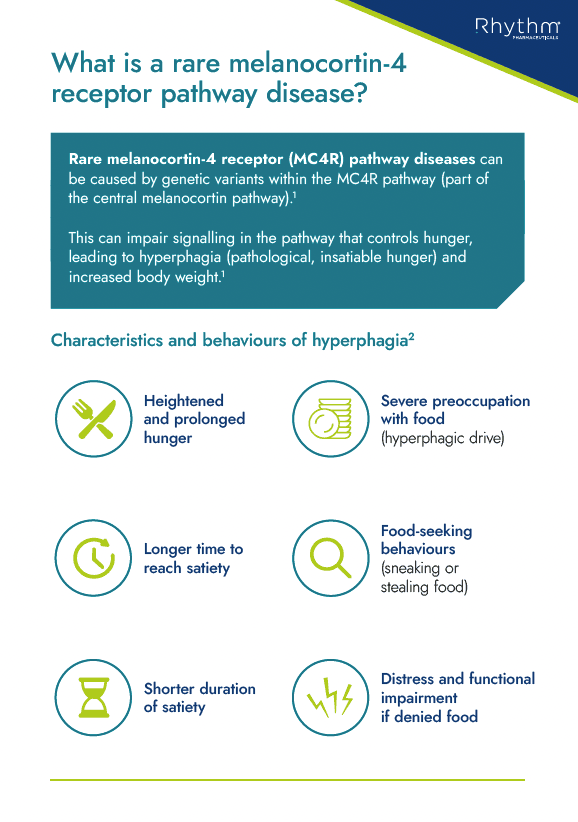
Educational information about hyperphagia, including its characteristics and behaviours and its association with rare MC4R pathway diseases
Handout
References:
- 1. Yazdi FT, et al. PeerJ. 2015;3:e856.
- 2. Acosta A, et al. Genes Nutr. 2014;9:384.
- 3. Huvenne H, et al. Obes Facts. 2016;9:158–73
- 4. Forsythe E, et al. Orphanet J Rare Dis. 2023;18:12.
- 5. Pomeroy J, et al. Pediatr Obes. 2021;16:e12703.
- 6. Beales PL, et al. J Med Genet. 1999;36:437–46.
- 7. Forsyth R, et al. Bardet-Biedl Syndrome Overview. 2003. Available at: https://www.ncbi.nlm.nih.gov/books/NBK1363/ [last accessed: February 2024].
- 8. Styne DM, et al. J Clin Endocrinol Metab. 2017;102:709–757.
- 9. August GP, et al. J Clin Endocrinol Metab. 2008;93:4576–99.
- 10. Kleinendorst L, et al. BMJ Case Rep. 2017;2017:bcr2017221067.